About the System: Judicial vs. Legislative Pathways

Recently, solicitors with experience representing health practitioners against professional services review have given an opinion that there is unfairness “baked into the legislation” governing the legal PSR process. This means that obtaining justice through a court appeal is almost impossible. Some practitioners have won their appeal, and then learn that the HIC or AHPRA are not bound to accept these decisions. In short there is no judicial pathway to justice to appeal any decisions against doctors, available to doctors.
The solicitors have commented that there are no other equivalent schemes to the PSR in any other profession. For example, you would never see a lawyer required to repay all the legal services they have undertaken for the last two years on behalf of a client. It seems uniquely unfair to require the doctor to repay money when the doctor may have obtained No benefit from their actions (such as in the case of ordering some “limited” pathology tests for the benefit of their patients).
There have been cases frequently in this regard where the doctor has been required to repay the HIC for all the tests they have ordered for which the patient is the beneficiary. Also there has been a requirement for the doctor to repay all their earnings even when they have not received all these earnings, (such as in the case of an employer collecting their administrative percentage from the doctor prior to paying the doctor). This situation is an anathema in considering that the practice may have made the mistake in billing, not the doctor. Yet the doctor is liable for compensating the government in full for the mistakes of other parties.
The correct action is to require the “patient’ to repay the benefits since they are the beneficiary of the medical procedures/ testing. Pathology processed the requests without asking the patient for payment of “unjustified” medical tests. Pathology did not require the provision of history or seek history which would have verified the Medicare rebatability of the ordered pathology tests.
The government is avoiding asking the patient for money since this is a real vote loser.
So who made the doctor responsible for any errors re benefits in the scheme. Why would any sane person accept such a role without copious compensation and significant “compliance” funding to allow them to do all the checks and work to allow all restrictions to be met. It’s just something else lumped on doctors, especially stupid bovine GPs- the requirement to do an inadequately funded consultation without no appreciation of the “time” demands of meeting the constraints imposed.
Some of solicitors involved have even opinioned that they have not seen any practitioner who has actually done anything deliberately “wrong” medically. It is usually the technical aspects relating to medical administration or records which earn the doctor the conviction and the reprimand, rather than any deliberate scheme to defraud the government.
In appealing through the legal system against a decision made against a doctor (the judicial pathway), must needs focused on a technical, legal argument about whether the process was in breach of rules within the legal system. There is no allowance for a focus on the merits or facts of the case. (This is usually the primary focus of the doctors – not the legal technicalities). It can take years to appeal such a judgement and requires reference to many (case law) events spanning over many years which a solicitor would judge to be relevant to the case in process.
Grounds for appeal which have been used by litigants confronting the PSR in the past include:
1. Natural justice/procedural fairness:
o trying to answer the question of whether the process has to in fact afford a person procedural fairness or not
o whether the person was given what is characterised as a “fair hearing”
o Whether there was any element of “bias”.
2. Relevance:
o Were irrelevant issues taken into consideration and relevant issues ignored? That is, non-existent rules nowhere to be found in the legislation but created by peers/director
o Were expert opinions ignored that say the billing practice is completely acceptable?
3. Reasonableness:
o Would a reasonable person looking at the decision and process say it is extremely unreasonable? Examples: Is it reasonable to ask a GP registrar to pay back half-a-million dollars when they saw probably only a quarter of that money or less and was under the direct supervision of a training provider?
o Is it reasonable to expect a semi-retired specialist to be smacked with million-dollar fines- money they never earned in the first place, virtually driving them into bankruptcy at the very end of their career?
4. Implied Political Freedom:
o Is there vital information withheld from the general public that would influence the way people will vote for the government; that is, Section 106ZR secrecy clause?
Would the general public feel uncomfortable knowing how their GPs are getting interrogated and prosecuted for providing them with essential services?
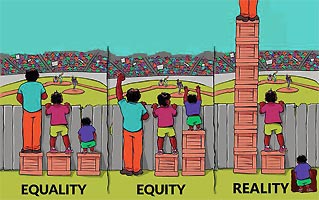
The opinion is that the system is broken – in the way it was set up in the first place. It needs to be replaced with something more equitable and fairer. And this brings us to the need for alternatives to the existing process. This requires the crafting of suitable legislation (a “bill”), which is passed through Parliament, changing the law.
Senate enquiries and Royal Commissions do not change the law. They can come up with recommendations for change in the law. But they do not craft new legislation. They do not propose new legislation. And they can be ignored at the whim of the government of the day.
The government has the power to completely ignore them .Both AHPRA and PSR have had Senate inquiries into their processes and some things may have changed, but not much.
The legislative process is divided into seven stages:
1. Presentation, explanatory speech and first reading
2. Committee consideration
3. Committee report
4. Second reading
5. Consideration-in-detail
6. Third reading
7. Royal Assent
Once we hit stage seven, the proposal or bill becomes a piece of law.
How do we create new laws? We contact one or two MPs (federal) in each state and territory, preferably a mix of opposition and ones in power. We give them a draft bill that we create after input from aggrieved individuals and advice from our legal team. Then these MPs will, once convinced, proceed through these stages for us and fight to get this tabled into the
Dr Karmakar has suggested his next step for political action? Doctors need a united a front to create these changes. Join AHPAS today to join Dr Karmakar’s political action group and email info@ahpas.com.au to help us create this change. He suggests that you can join as a standard member for free, or pay a nominal fee towards your membership that will be used to fund and run these lobbying activities.
Dr Karmakar’s Solution: Judicial litigation may take a lot of money and time, but collegial lobbying and advocacy run by professionals does not. It is always a better and preferred way, so let’s make it happen!
All it takes is a bunch of colleagues with intelligence and grit. If that is you contact him to be part of his team. This site promotes a large range of other actions to create change. It’s an isolating path to be on, so any help would be appreciated to draft new bills and find the right MPs.
Dr Karmakar is the founder and CEO of AHPAS (Australian Health Practitioners Advisory Solutions).
This site is about other alternative actions: essentially Union action in the progressing of the aim of limiting the reach of AHPRA and limiting its actions against doctors.
The most common avenue for doctors judged to have breached medical professional standards is to appeal the finding in a state Civil and Administrative tribunal e.g. NSW CAT (NSW), e.g. QCAT (Qld).
The appeal has time limitations for lodgement which are quite tight (usually 30 days), considering that most AHPRA investigations have run for 6 months to 2 years.
The appeals can only be made on specific grounds.
Medical Defence Organisation will not fund them as they regard any appeal as unwinnable. So in spite of indemnity medical defence insurance, you will be paying for all of it yourself, organising it yourself and working with solicitors who are delusional in the belief that the opposing party (AHPRA) is willing to negotiate or to reconsider its actions in any way.
I will present the QCAT process below because we need doctors to stand up for themselves and the QCAT appeal actions are actually part of our campaign for limiting AHPRA and its powers.
QCAT Appeal Criteria
Appeal on Point of Law / Point of Fact
AHPRA amended the "complaint" / "indictment" of the patient. Amendment doees not relate to the "offense" as listed on the indictment.
AHPRA Board presented own opinion as "evidence" for decision.
No evidence was requested from applicant.
AHPRA investigator failed to show evidence for or against the matter.
Substituted amended indictment prejudiced applicant's ability to defend the case.
Patient commited an offence during the course of their complaint; preventing practitioner from making the record, engaging in illegal activities.
All QCAT hearings are digitally recorded in compliance with the Recording of Evidence Act 1962.
To order an audio recording or a transcript (a written record of what was said in a hearing), contact Auscript via clientservices@auscript.com.au or 1800 287 274 (8am - 6pm AEST).
You can request reasons for a decision within 14 days of the decision. If you are unable to access an audio copy of reasons (e.g. if you have a hearing impairment) please advise the registry when requesting reasons.
Forms to Use
form-22-app-ref-disciplinary-proceeding.pdf
form-23-app-review-decision.pdf
Form-58-Notice-of-withdrawal-of-application-or-referral.pdf
The Medical Legislation If You Are Keen:
Health Practitioner Regulation National Law act-2009-045.pdf
 No More. It Ends Here.
No More. It Ends Here.